Dark Circles Under the Eyes: A Major Concern for People with Black, Brown, and Mixed Skin
Dark circles under the eyes are one of the most common aesthetic concerns, regardless of skin type. However, in black, brown, and mixed skin, they are often more pronounced, persistent, and particularly difficult to correct. This specificity is explained by the unique structure of the eye contour and by the tendency of black, brown, and mixed skin to develop dark spots as a symptom of any dermatological problem. Before treatment, it is essential to distinguish the real causes (pigmentary, vascular, structural) and to tailor care to the specificity of black, brown, and mixed skin.
What characterizes the periocular area?
The area around the eyes is particularly fragile as it is thin: 2 to 4 times thinner than the rest of the facial skin. It is poorly protected and less resilient; it is the most sensitive skin on the face.
The hydrolipidic film is less abundant than on the rest of the face (sebaceous and sweat glands are less numerous), so the protection against external aggressions is reduced, as is protection against dehydration.
The epidermis is very thin in this area, which also makes the skin more vulnerable. The slowing of cellular renewal and lipid synthesis (responsible for hydration) results in less efficient cells (poorer cell adhesion), leading to thinning of the epidermis and diffusion of intrinsic water to the surface.
The dermis is also thinner. It is depleted in collagen and elastin fibers. Beneath the skin, the tissue is very loose, making it easily stretchable.
In the hypodermis, there are few adipose cells, and water reserves are low, so the skin dries out, becomes fragile, and becomes a prime site for wrinkle formation. The eye contour is particularly rich in blood vessels; however, this area can easily suffer from circulation disorders due to poor lifestyle habits. Indeed, when lymphatic and blood circulation slows down or becomes congested, an accumulation of micro-waste products and toxins occurs, which appears through the very thin epidermis as dark circles. Poor cellular exchanges also cause water retention, the eyelids swell, forming under-eye bags.
The area is rich in muscles, 22 in total, 14 of which are in constant motion: blinking every 10 seconds (more than 10,000 times a day) to ensure continuous corneal hydration. This essential function of the eyelids is only possible due to the thinness of the skin; however, with 10,000 blinks a day, fibers are more rapidly deteriorated and become less firm, so the eye contour is the first area to show fatigue and signs of aging: dark circles, bags, and fine lines.
The skin around the eyes is highly reactive due to its richness in inflammatory cells (mast cells); this explains frequent intolerance and allergy reactions.
All these specificities contribute to the sensitivity of the eye contour, especially when exposed to overly irritating cleansing or inappropriate cosmetic products, such as those containing allergenic actives or fragrance. These daily micro-aggressions sometimes trigger allergic reactions, making the eye contour the first area of the face to show signs of aging.
The most common periocular issues
Eyelid swelling: Swelling of the eyelids appears as a result of decreased lymphatic microcirculation.
Bags: Under-eye bags are caused by disruptions in water flow. With age, the 10,000 blinks per day eventually weaken the support fibers of the eye contour, and the skin relaxes. Additionally, blood and lymphatic vessels, which nourish cells in this area, slow down. Poor cellular exchanges induce water retention, causing eyelids to swell and form under-eye bags.
Fine lines, wrinkles: Wrinkles and fine lines result from repeated eye folding and the degradation of dermal fibers linked to physiological and photoaging.
Dryness, atopic dermatitis, eczema…: These discomforts are related to a deficiency in the hydrolipidic film present on the periocular skin.
Ptosis: Eyelid ptosis (drooping eyelids) is caused by muscular and skin relaxation due to aging.
Fat deposits: Fat deposits around the eyelids often reflect a disorder in lipid and cholesterol metabolism.
Irritation, redness, tingling: These phenomena usually occur due to allergies to inappropriate or misused products.
Dark circles: Dark circles are mainly linked to pigmentation disorders of the skin and fragile capillaries. Indeed, decreased microcirculation makes blood vessels darker, more pronounced, and more visible. With less elastic and less watertight vessel walls, blood leaks from capillaries into the interstitial space. Hemoglobin then accumulates in the infraorbital area and oxidizes into biliverdin, bilirubin, or iron, causing the characteristic bluish coloration of dark circles. Moreover, if lymphatic drainage is impaired, the elimination of pigments under the skin cannot occur properly.
We distinguish:
- Hollow dark circles: They hollow out the lower eyelid, giving a “sunken” appearance. They are caused by fat loss in the eyelid or facial aging: the skin thins, cheekbones flatten, and the face appears “skeletal.”
- Full dark circles: The opposite situation occurs; the eyelid appears “full” due to orbital fat herniation, permanently distending the lower eyelid skin. This differs from puffed eyes in the morning (lymph accumulation during the night, which disappears after getting up).
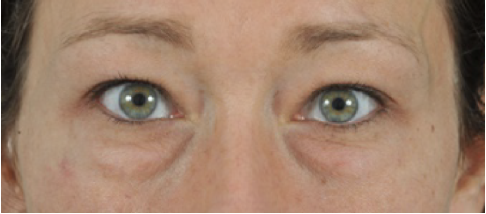
- Pigmentary dark circles: Characterized by more or less intense pigmentation of the lower eyelid. The color varies and can have different origins. In fair-skinned individuals, dark lower eyelids often result from accumulated melanin. Generally hereditary, this type appears brown or even bluish. Conversely, in black, brown, or mixed-skinned individuals with high melanin concentration on the eyelids, the coloration extends across all four eyelids to the lash line. Here, the dark circle color is noticeably more intense than the surrounding skin, ranging from dark brown to black.
- Thin eyelid skin revealing subdermal capillaries: The dark circle, called “vascular,” appears blue or red.
- Conversely, individuals with thick eyelid skin (stratum corneum) or large fat deposits: the dark circle takes on a yellow color.
- Mixed dark circles: This corresponds to a combination of the above abnormalities: hollow or puffy, varying pigmentation, excess skin, presence of wrinkles.



Periorbital Hyperpigmentation (POH): Focus on Black, Brown, and Mixed Skin
POH is generally benign, extremely common but poorly defined, with very limited scientific data on its clinical profile and pathogenesis. This hyperpigmentation is known as “pigmentary dark circles,” “pigmentary spots,” or “infraorbital darkening.” Aesthetic concerns of the face have been the main reason for dermatological consultations in recent years. POH is defined as homogeneous, bilateral hyperchromic macules, mainly affecting the lower eyelids but sometimes extending to the upper eyelids, eyebrows, malar regions, temporal regions, and lateral nasal root.
Clinically, POH presents as light-to-dark brown or brown-black pigmentation around the eyelids, giving the patient a tired appearance. POH prevalence is estimated at 30.76%. The onset is usually after puberty or in early adulthood (16–25 years). Genetic conditions are not necessarily congenital (present at birth); however, POH is often observed in multiple family members. The genotype is fixed at conception, but the phenotype may not manifest until adulthood. In such cases, penetrance is age-related, confirming that POH onset for most patients occurs in early adulthood.
POH is more pronounced in certain ethnic groups, particularly black, brown, and mixed-skinned individuals. Although it is not rare in men, women are more affected due to hormonal factors. Few statistics provide the frequency of its occurrence, but judging by the number of cosmetic products marketed to treat it, dark circles are a cosmetic concern for many individuals. It is absolutely essential to define the type of periocular hyperpigmentation and determine causal factors to direct appropriate measures for the best results.
Researchers recently performed a clinical analysis and proposed a classification based on pigmentation structure and vascularization. Periorbital hyperpigmentation is classified as pigmentary (brown color), vascular (blue/pink/purple), and mixed type based on their combination.
The mixed type (M) includes four subtypes: pigmentary-vascular (PV), pigmentary-structural (PS), vascular-structural (VS), and a combination of the three. This mixed type combines two or three of the appearances described above.
The pigmentary type (P) appears as a brownish infraorbital tint.
The vascular type (V) appears with blue, pink, or purple coloration with or without periocular swelling.
The structural type (S) appears as structural shadows formed by the anatomical contours of the face. It may be associated with infraorbital eyelid bags, blepharoptosis (drooping of the upper eyelid due to traumatic lesion), and fat loss with bony prominence.
Periorbital hyperpigmentation presents one or more of the following characteristics:
- Diffuse and concentrated melanin deposits,
- Superficial, slowed subcutaneous vascularization,
- Shadows caused by orbital fat.
There is very limited scientific data on the clinical profile and pathogenesis of POH. Various exogenous and endogenous factors may be involved in its pathogenesis.
The table below provides a comprehensive view of the different causes of dark circles.
| Endogenous | Exogenous |
|---|---|
| Genetics / heredity | Fatigue |
| Slowed vascularity and location | Slowed vascularity and location |
| Advanced age | Post-inflammatory hyperpigmentation secondary to atopic and contact dermatitis |
| Vitamin K deficiency | Hormonal therapy (oral estrogen contraceptives) |
| Thin skin | Wearing glasses |
| Exhaustion of periocular muscles | Stress |
| Periocular edema | |
| Increased alpha-MSH secretion via HHS axis | |
| Increased alpha-MSH secretion during pregnancy | |
| Menopause |
Endogenous factors of dark circles
POH is considered to have a genetic basis. Multiple family members are generally affected by periocular hyperpigmentation. Many report pigmentation recognized in early childhood, which increases with age. Genetics therefore play a role in dark circle appearance. Additionally, the thinness of the skin under the eyes is also hereditary.
In cases of fatigue, insomnia, or crying, blood vessels in the lower eyelid dilate, and circulation slows, causing dermal extravasation of blood. The release of ferric ions locally generates free radicals, stimulating melanocytes and producing melanin pigmentation. Superficial vascularization through thin skin is a frequent cause of POH, especially when circulation is slow in the periocular area. This condition usually affects all lower eyelids with a purplish appearance due to deep blood vessels covered by a thin layer of skin.
Dark circles tend to become more visible and permanent with age. This occurs due to aging and collagen loss; skin loses elasticity and becomes more sensitive. Blood vessels in this area then widen and swell, becoming more noticeable.
Vitamin K is a common ingredient in creams used to treat under-eye aging and problems, including dark circles. Vitamin K acts as a coagulant, helping to strengthen blood vessels and prevent damage. Vitamin K deficiency can lead to capillary rupture, dermal blood extravasation, and formation of under-eye dark circles. Thinner skin in this area makes the blood more visible. Indeed, some individuals have thinner skin than others, increasing the risk of dark circles.
Research has shown that exhaustion of periocular muscles can play an important role in POH. Muscle fatigue reduces tonicity, causing capillary dilation and dark circle formation.
Abnormal fluid accumulation around the eyes, called periocular edema, gives the appearance of dark circles. Periocular edema may indicate certain diseases, such as mononucleosis or Basedow’s disease (hyperthyroidism)…
Keratinocyte-derived agents whose production is stimulated by UV include adrenocorticotropic hormone (ACTH) and alpha-melanocyte-stimulating hormone (α-MSH, produced from ACTH cleavage), the most potent melanogenesis activators. During stress, the adrenal gland secretes significant cortisol (allowing the body to resist stress), but prolonged stress can deplete the adrenal gland, causing hormonal imbalance. ACTH then increases to stimulate cortisol production. Dark circles result from elevated ACTH, which cleaves into α-MSH, stimulating melanin secretion.
During pregnancy, sex steroid hormone production increases due to placental chorionic gonadotropin. Consequently, adrenal and pituitary secretion of melanocyte-stimulating hormone (MSH), thyroid-stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), and glucocorticoids rises. ACTH cleavage into α-MSH stimulates melanocyte activity, contributing to gravidic pigmentation affecting the armpits, breasts, inner thighs, and anogenital area. Increased TSH also induces endocrine changes by enhancing thyroid activity, causing either diffuse hyperpigmentation or periocular hyperpigmentation. Additionally, hormone level changes during pregnancy can dilate small blood vessels, making under-eye dark circles more visible.
During menopause, skin loses density, sebaceous glands cease activity around age 50, causing skin relaxation. Estrogen and progesterone gradually decrease, leaving testosterone (present in all women) unopposed, causing facial vascular disturbances and potential dark circle formation.
Exogenous factors of dark circles
Lack of sleep can pale the skin, making circulating blood more visible and darker. Sleep apnea may also contribute to dark circle formation. Smoking and alcohol are risk factors. Slowed lymphatic circulation during peak activity may explain this.
Contact eczema is an allergic eczema (contact allergic dermatitis). It appears 2–72 hours after exposure to a substance: an allergen. It is an immunological hypersensitivity that, once acquired, is usually permanent. Unlike atopic dermatitis, it has no genetic origin. Contact eczema is particularly marked where the allergen contacts the skin, but can extend and even generalize. Sources include cosmetics, medications, or allergens.
Atopic dermatitis or eczema denotes chronic and/or recurrent inflammatory skin manifestations associated with atopy, a highly prevalent polygenic hereditary trait, with clinical manifestations (atopic dermatitis, allergic rhinitis, asthma) affecting about one-third of the general population. POH can therefore result from rubbing and scratching around the eyes and fluid accumulation due to allergy, as in atopic or contact dermatitis.
Hormone intake via oral contraceptives can decrease steroid sexual hormones due to slowed gonadal gland activity. This slowdown may lead to hypothyroidism (reduced thyroid activity), putting the body in a catabolic state. Many hypothyroidism symptoms are similar to adrenal fatigue, as thyroid and adrenal glands work together to maintain metabolic balance. Their insufficiencies often co-occur, causing symptoms including dark circles, hyperpigmentation of sun-exposed regions, and thinner, drier skin. Additionally, estrogen-based pills increase blood coagulation factors and reduce anticoagulant factors. This change causes pro-coagulation, potentially forming dark circles due to poorer blood circulation combined with thin periocular skin.
Wearing glasses can cause micro-traumas to the lower eyelids. Repeated over time, this induces inflammatory phenomena and vascular or pigmentary spots.
Stress and anxiety can damage the body both psychologically and physically. Causes of stress are numerous, and susceptibility varies among individuals; genetics also plays a role. Prolonged, poorly managed stress can lead to fatigue, irritability, burnout, depression, and skin problems. Physically, stress can trigger dark circle formation.
Dermocosmetic management adapted to dark circles on black, brown, and mixed skin
- Hygiene and protection: Gentle cleansing without harsh surfactants, avoiding rubbing, and applying daily sun protection (SPF ≥ 30).
- Depigmenting, non-irritating actives: Prefer gentle actives such as niacinamide, N-acetyl glucosamine, oligopeptide-68, and wheat bran extract. These ingredients slow melanogenesis without irritating thin periocular skin.
- Circulatory and anti-fatigue actives: Caffeine, hesperidin, vitamin K, and biomimetic peptides stimulate microcirculation and strengthen capillaries, while hyaluronic acid hydrates and plumps.
- Application technique: Apply a small amount morning and evening with gentle tapping from the inner to outer eye. Keep the product refrigerated for an immediate refreshing effect.
- Complementary dermatological solutions under medical supervision: Gentle mandelic acid peels, carboxytherapy, or Q-switched laser may complement management, under strict dermatological supervision, especially on black, brown, and mixed skin.
- Prevention and maintenance: Adequate sleep, hydration, sun protection, avoiding rubbing, and regular use of products adapted to pigmented skin are key for effective prevention.
In conclusion
Dark circles on black, brown, and mixed skin are multifactorial. Their reduction requires precise diagnosis, an adapted dermocosmetic routine, and daily prevention. Formulations combining niacinamide, N-acetyl glucosamine, and draining peptides provide visible results without irritating this fragile area.






