Melasma & Black Skin
Specificities and Treatments of the "Pregnancy Mask"
Melasma on black skin - illustration image
Melasma is characterized by irregular brown pigmentation on the face. It is most often localized in the cheeks, in the form of a mask, and of secondary appearance to hormonal impregnation, hence its popular name " pregnancy mask" (chloasma). Common in populations with black, matte and mixed skin, this pathology is benign but displaying, highlighting an aesthetic damage that must be corrected.
" Melasma ", from the Greek " melas " meaning black, is a skin pathology characterized by the appearance of excessive pigmentation in the photo-exposed areas, especially the face. Although it can affect men, melasma is more frequently found in women through the preponderant role of hormonal impregnation.
The topography of the lesions is variable, there are 4 preferential locations classified below in order of frequency:
- centrofacial : cheeks, forehead, chin, upper lip
- malary : symmetry in the cheeks and nose
- mandibular : lip and chin
- maxilla : upper jaw
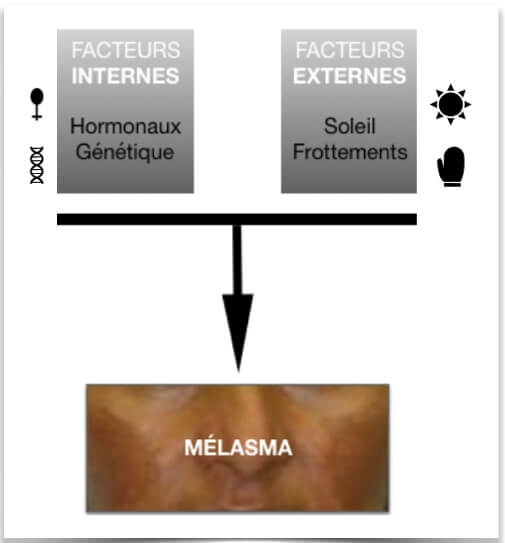
Origin of dermatosis
The role of female hormones is mostly questioned. Indeed, the increase in the concentration of estrogen and progesterone during pregnancy, the use of an oral contraceptive or during a menopausal replacement therapy is very frequently associated with the appearance of melasma. The biological effects of these two types of hormones are mediated by two distinct receptors whose expression increases in melasma patients.
However, in humans, the endocrine cause is rejected and the occurrence of this dermatosis is not yet resolved.
Finally, because of the family and ethnic character, a genetic terrain seems to be possible.
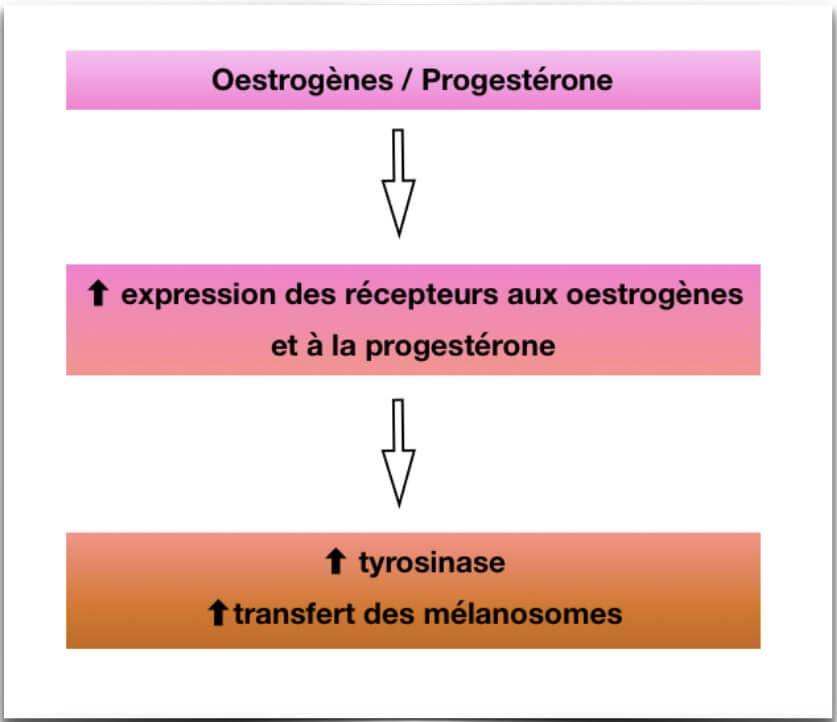
If an internal factor is necessary, it is the external factors that trigger the synthesis of pigments (melanogenesis) and therefore the revelation of skin signs. These include:
• sun exposure. The effect of UVs on melanogenesis is well established: they stimulate this physiological process leading to an increase in the content of melanin, responsible for the dark color of the skin. However, an excessive deposit of melanin in the epidermis and dermis has been observed at the microscopic level in patients with melasma. In addition, epidemiological studies suggest that sun exposure alone or sun exposure during pregnancy can trigger or worsen melasma lesions. Moreover, this pathology has a peak during the summer and there is a lightening of the spots during the winter.
• local microtraumas, type of friction when toileting. Indeed, melanocytes, cells of the body responsible for the brown color, are called " mechanosensitive ", that is to say that they are stimulated as a result of mechanical frictions. In addition, contrary to what one might think, dark skin is more sensitive than light skin and therefore requires particularly gentle care to avoid this hyperpigmentary stimulation.
Transient in light phototypes, melasma is most often a chronic disease that persists or even worsens over the years on dark skin. The treatment is very effective in reducing hyperpigmentation almost completely.
If the spot evolves (change in color, size, presence of relief) or causes discomfort (tingling, burning, pruritus), do not hesitate to consult a dermatologist to rule out any potentially malignant dermatoses.
Care protocol
1. Eradication of external factors
• Sun protection is essential, in prevention (during pregnancy for example) but also to avoid aggravating a melasma already installed. Sun exposure, even short, can lead to a darkening of the lesions that will take months to go. Favor sidewalks in the shade, lunches in shaded terraces, umbrellas at the beach. Do not hesitate to wear a wide-brimmed hat and sunglasses. In addition, My SUN'OYA® SPF 50 Solar Fluid has UVA protection and SPF50 that effectively protects against UVB radiation. Its 0% white trace technology is suitable for dark skin. It is to be used daily in sunny weather, every 2 hours if the exposure is intense.
• to avoid attacking the skin of the face by a toilet too energetic, the LABORATORY IN'OYA advises you to use My Micellar Water " Sensitive Skin" CLEAN'OYA® to apply on a cotton pad. It gently cleanses and removes makeup and soothes the skin thanks to bisabolol, a powerful plant active ingredient. A gentle exfoliation can also be done once a week to complete the skincare routine. My CLEAN'OYA® EXTRA " Exfoliating Cleanser" Gel uses bamboo microbeads and a chemical exfoliation based on salicylic acid to regenerate the skin without attacking it and to promote the gradual elimination of the hyperpigmented epidermal layer.



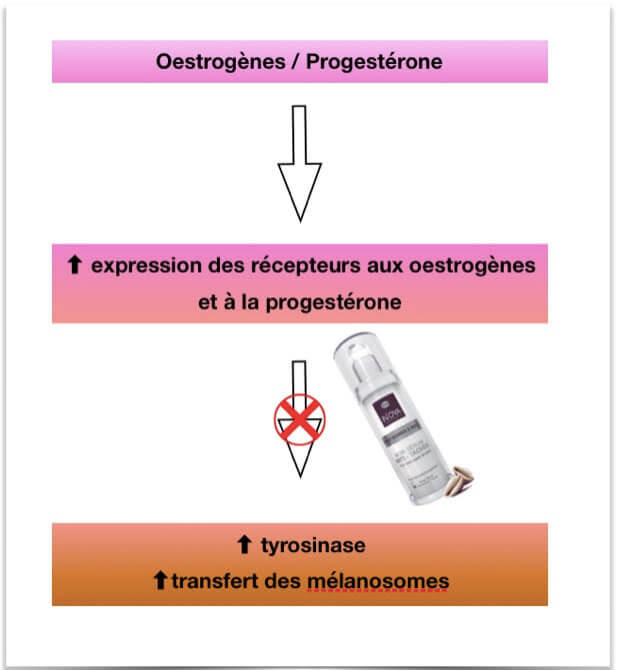
2. Unifying treatment
This should be initiated only after stopping hormonal impregnation. The IN'OYA laboratory has developed My MEL'OYA ® anti-stain serum specifically adapted for pigmented skin since it acts at two physiological levels: it prevents the transport of melanosomes and inhibits the synthesis of melanins (action on the enzyme tyrosinase).
A lack of results after 6 months of use must require an adaptation of the protocol: it will be necessary to ensure the eviction of triggering factors (sun exposure, aggressive toileting, hormonal impregnation) and consider a dermatological consultation.
Other physical and chemical means, more aggressive, are also available but rigor is required because a risk of secondary hyperpigmentation can appear and aggravate the initial hyperpigmentation. These techniques require the advice of a dermatologist and should not be performed in an innocuous manner.
Finally, some so-called "dermal " melasmas cannot be treated at this time. Only dermatological examination can highlight this type of melasma, which remains rare compared to the epidermal melasmas mentioned above.